Here’s an overview:
Introduction to Caesarean Section
A Caesarean section, also known as a C-section, is a surgical procedure used to deliver a baby through incisions made in the mother’s abdomen and uterus. This procedure may be planned in advance or performed when unexpected complications arise during childbirth.
Reasons for a C-Section
- Medical Complications: Pre-eclampsia, infections, or chronic conditions.
- Fetal Distress: Irregular heart rate or other indications of distress.
- Labor Complications: Prolonged labor or stalled labor progression.
- Multiple Pregnancies: Twins, triplets, or more.
- Previous C-Section: Previous deliveries via C-section could necessitate another one.
Understanding the indications for a C-section is crucial for expectant mothers.
History and Evolution of C-Section
The origins of the Caesarean section date back to ancient times, although initially performed post-mortem for maternal death. It evolved with surgical advancements over centuries.
Key Milestones:
- Ancient Rome: Named after Julius Caesar, though he was not born this way.
- 16th Century: First successful C-section with mother’s survival documented.
- 19th Century: Introduction of anesthesia and antiseptic techniques.
- 20th Century: Advances in surgical methods and antibiotics drastically reduced mortality rates.
- 21st Century: Modern C-section practices emphasize maternal and neonatal safety, with minimally invasive techniques.
Transition from emergency procedure to elective option reflects medical advancements and changing views on childbirth.
Medical Indications for a C-Section
A C-section might be medically necessary for various reasons, including emergencies. Common indications include:
- Fetal distress: When the baby exhibits signs of distress, prompting immediate delivery.
- Placenta previa: The placenta covers the cervix, posing a risk during vaginal birth.
- Umbilical cord prolapse: The cord slips into the birth canal before the baby.
- Breech or transverse positions: The baby is not in a head-down position.
- Multiple pregnancies: Complications arise with twins or more.
- Pre-existing health conditions: Maternal conditions like hypertension or diabetes.
- Previous C-section: Previous cesarean delivery increases the risk of complications with vaginal birth.
Preparation for a Caesarean Section
Preparation for a Caesarean section involves several critical steps. Expectant mothers should follow a detailed checklist to ensure readiness.
Medical Preparations:
- Blood Tests: Ensure to complete blood work as instructed.
- Medications: Discuss any medications being taken, including supplements.
- Fast: Abstain from eating or drinking for at least 8 hours before the surgery.
Personal Preparations:
- Hospital Bag: Pack essentials such as comfortable clothing, toiletries, and baby items.
- Birth Plan: Communicate birth preferences with healthcare providers.
- Support System: Arrange for a partner or family member to be present.
Informed, organized preparation can help alleviate stress and ensure a smoother experience.
The Surgical Procedure: Step-by-Step
- Pre-Operative Preparations
- Hospital staff assists the patient in changing into a surgical gown.
- An IV line is inserted for medication and fluids.
- Anesthesia is administered, usually spinal or epidural.
- Initial Incision
- A horizontal incision is made in the lower abdomen.
- The incision is approximately 10-12 cm long, just above the pubic hairline.
- Uterine Incision
- A similar horizontal incision is made in the uterus.
- The doctor carefully opens the uterus to access the baby.
- Delivery of the Baby
- The baby is gently lifted out.
- The umbilical cord is clamped and cut.
- Post-Delivery Procedures
- The placenta is removed.
- Incisions are closed with sutures.
Types of Anesthesia Used in C-Sections
1. Spinal Anesthesia:
- Injected directly into the spinal fluid.
- Provides quick and effective pain relief.
- Numbs the body from the abdomen down.
2. Epidural Anesthesia:
- Administered into the epidural space around the spinal cord.
- Can be adjusted for prolonged procedures.
- Allows the mother to stay awake and experience birth.
3. General Anesthesia:
- Used in emergency situations or when spinal/epidural are not suitable.
- Induces complete unconsciousness.
- Offers immediate pain relief but involves more risks.
Each type has specific indications, advantages, and potential side effects. Consulting the healthcare provider to choose the most appropriate option is crucial.
Risks and Complications Associated with C-Sections
Cesarean sections, like any major surgery, carry several risks and potential complications. These may include:
- Infection: Post-operative infections can occur at the incision site, in the uterus, or other pelvic organs.
- Blood Loss: Increased risk of excessive bleeding and complications such as anemia.
- Blood Clots: Higher risk of developing blood clots in the legs or lungs.
- Reactions to Anesthesia: Adverse reactions to anesthesia, including nausea and severe headaches.
- Surgical Injury: Possibility of accidental injury to nearby organs such as the bladder or intestines.
- Future Pregnancies: Increased likelihood of complications in future pregnancies, including uterine rupture or placental issues.
Recovery Process: What to Expect Post-Operation
Post-operation, mothers will initially stay in a recovery room. Medical staff monitor vital signs, including heart rate and blood pressure. Pain management is crucial, with options such as epidural, spinal, or oral pain relief. Within a few hours, the mother may begin to move slowly.
Key Stages of Recovery:
- Immediate Post-Op: Vital signs monitored, pain management.
- First 24 Hours: Catheter removal, encourage walking.
- First Week: Manage pain, monitor incision site, gradual mobility increase.
- First Month: Regular follow-ups, avoid heavy lifting, focus on nutrition and hydration.
Recovery time varies; always follow medical advice.
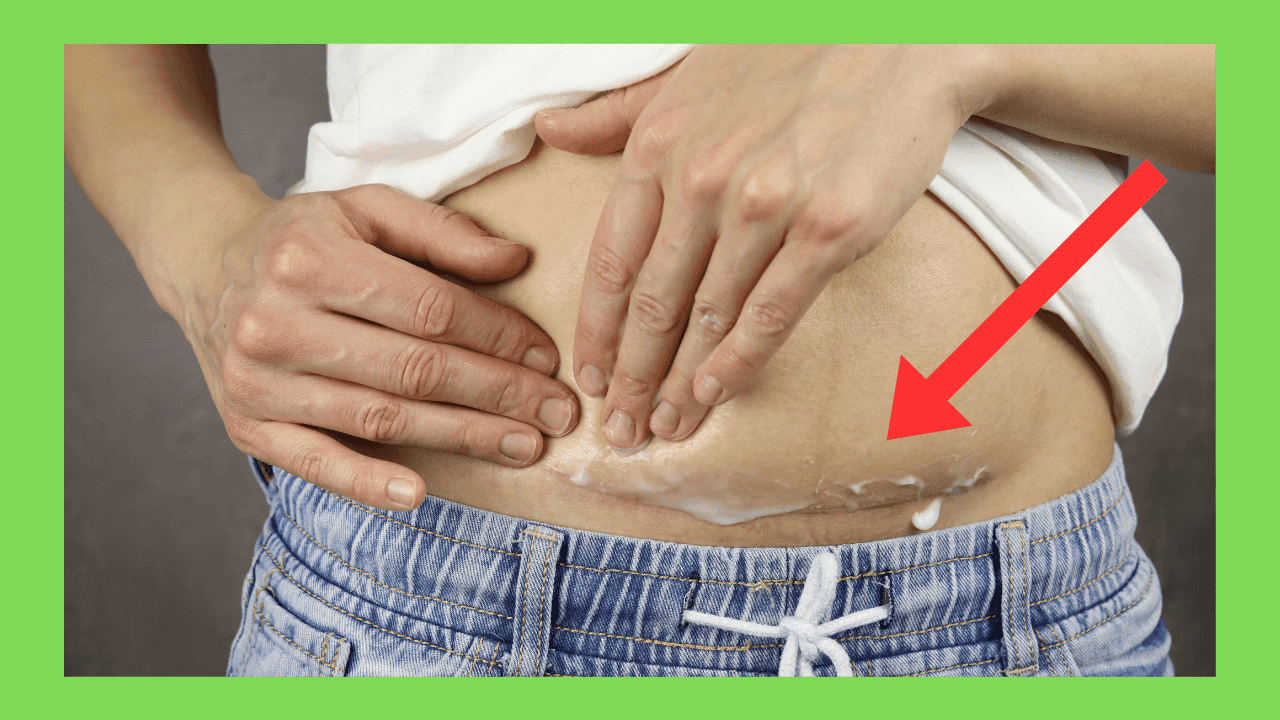
Caring for Incision and Pain Management
- Keep the Incision Clean and Dry:
- Wash hands thoroughly before touching the incision.
- Use mild soap and water to clean the area gently.
- Pat dry with a clean towel; avoid rubbing.
- Monitor for Signs of Infection:
- Redness, swelling, or heat around the incision.
- Unusual discharge or odor.
- Increased pain or fever.
- Pain Management:
- Follow the prescribed pain medication schedule.
- Use over-the-counter pain relief if permitted by the healthcare provider.
- Apply a cold compress to reduce swelling.
- Avoid Strain and Heavy Lifting:
- Do not lift anything heavier than the baby.
- Avoid strenuous activities until clearance from the doctor.
- Wear Comfortable, Loose-fitting Clothing:
- Choose cotton garments that do not irritate the incision.
- Opt for high-waisted underwear to avoid pressure on the incision site.
Consult a healthcare provider if experiencing severe pain or infection signs.
Emotional and Psychological Impact of a C-Section
Undergoing a C-Section can vary greatly in emotional and psychological effects from person to person. The anticipation and recovery process might lead to various feelings that could include:
- Anxiety and Stress: Concerns about the surgery, recovery, and the baby’s health.
- Disappointment: If a vaginal birth was desired, feelings of disappointment or inadequacy may arise.
- Postpartum Depression: Hormonal fluctuations and the physical trauma of surgery can increase the risk.
- Relief: For some, planned C-sections bring relief from potential birthing complications.
- Bonding Issues: Initial recovery may impact the early bonding experience.
Importance of Postpartum Check-ups
Postpartum check-ups play a crucial role in ensuring the health and well-being of both the mother and the newborn. Essential reasons for these check-ups include:
- Monitoring Recovery: Assess the mother’s physical recovery from the Caesarean section, including incision healing and uterine health.
- Managing Complications: Early detection and treatment of potential complications such as infections, blood clots, or postpartum hemorrhage.
- Mental Health Screening: Evaluate and address postpartum depression or anxiety to provide necessary support and interventions.
- Breastfeeding Support: Guidance and assistance with breastfeeding techniques and addressing issues like mastitis.
- Family Planning: Discuss contraceptive options and future family planning.
Following these check-ups supports a healthy postpartum period.
Breastfeeding After a C-Section: Challenges and Tips
Expectant mothers should be aware that breastfeeding after a C-section can present unique challenges. Recovery from surgery, pain, and limited mobility may affect breastfeeding.
Common Challenges:
- Pain at the incision site
- Difficulty finding comfortable positions
- Delayed milk production
Tips for Successful Breastfeeding:
- Use Pillows: Support the baby and reduce strain on the incision.
- Stay Hydrated: Encourage milk production.
- Ask for Help: Seek assistance from nurses or lactation consultants.
- Skin-to-Skin Contact: Promotes bonding and stimulates milk flow.
- Rest Often: Ensures energy for feeding sessions.
Recognizing these challenges and implementing these tips can promote a more comfortable breastfeeding experience after a C-section.
FAQs About Caesarean Sections
What is a Caesarean section? A Caesarean section, or C-section, is a surgical procedure where a baby is delivered through an incision in the mother’s abdomen and uterus.
When is a C-section necessary? A C-section may be necessary for multiple reasons including:
- Complications during labor
- Health concerns for the mother or baby
- Multiple births (twins, triplets)
How long is the recovery period? Recovery from a C-section typically takes about 6-8 weeks. Hospital stays usually last 2-4 days.
Can someone have a vaginal birth after a C-section (VBAC)? Yes, many women can have a vaginal birth after a C-section, depending on their health and pregnancy circumstances.
Conclusion and Final Thoughts
Preparing for a caesarean section involves several critical steps. It is essential for expectant mothers to:
- Consult with healthcare providers.
- Understand the procedure and its risks.
- Prepare mentally and emotionally.
- Plan for postoperative care.
Proper planning helps mitigate anxiety and ensures a smoother recovery. Adherence to medical advice is paramount.
Effective communication with the medical team is crucial to address any concerns. Reading material, attending classes, and seeking support from experienced mothers can further aid in preparation. Prioritizing both physical and mental health is key during this period.